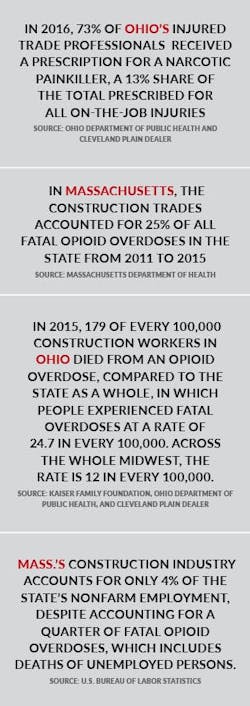
And that imbalance isn’t unique to Ohio.
Twenty-five percent of all opioid-related deaths in Massachusetts from 2011 to 2015 came from the construction industry, making workers six times more likely to die from opioids than those in any other industry. In some areas around Boston, construction workers accounted for nearly half of all opioid-related deaths.
Of course, opioids are not just a construction or remodeling problem, but a national issue. In the U.S., 47,600* people died of opioid overdose in 2017. You’re more likely to die from opioids in this country than a car crash.
But also, it is a remodeling problem.
Indiscriminate Attraction
I contacted Dr. Melissa Weimer to try to learn why a huge group of people, seemingly connected only by professional industry, might share an enhanced susceptibility to struggles with opioids. As medical director of the Addiction Medicine Consult Service at the renowned Yale New Haven Hospital in Connecticut, she was as good a bet as anyone to know.
Right away, Weimer acknowledged a higher risk for injury in trade professions that increases the likelihood of an opioid prescription—and resulting chances of dependency and addiction (two distinct issues). She also pointed out that males are twice as likely to die from an opioid overdose as females. As of 2018, men made up 90% of the construction workforce.
Yet experts caution against making assumptions. “It’s one of the misconceptions about addiction, that you might somehow be able to tell who would be likely to succumb to it,” says Weimer, who’s also an assistant professor at Yale University and board certified in both internal and addiction medicine. “It’s not about race, ethnicity, or socio-economic status. Addiction crosses all demographics, especially with opioids.”
Other types of drug abuse, such as cocaine, seem to have a weaker genetic tie. The current collective medical understanding of opioids is that more large-scale studies are needed to determine where on the genetic-component spectrum they belong.
Trauma, particularly childhood trauma, is another indicator. “An adverse childhood is a very strong indicator of potential risk in the future,” Weimer says.
The real trouble with profiling a potential addict or drug abuser is that what does indicate a predisposition to those behaviors, like genetics and childhood adversity, isn’t readily discoverable—at least not by an employer. Remodelers can’t very well pry into someone’s family history—that’s illegal.
Even if a company could obtain that private information, it wouldn’t necessarily help all that much. “Not everyone who lived through a traumatic childhood event is going to have a substance abuse disorder, and not everyone who didn’t experience trauma will be able to resist addiction,” Dr. Weimer says.
It’s the same with having a parent who drank, or in this case, abused opioids. It’s all so fuzzy.
It’s The Work
“It’s a big problem for our members,” says Reid Ribble, chief executive officer of the National Roofing Contractors Association, and a veteran roofer. “Opioids are a crisis. And it affects rural and suburban markets alike. We’re losing people all over.” Just this year a roofer confided to Ribble that he’d lost three employees to fatal opioid overdoses. The roofer didn’t want to discuss it on record.
Roofing has been hit hard by opioids, but so has all of remodeling. Power Home Remodeling Group, one of the largest exterior replacement contractors in the country, used the last year to collect data on how opioids were affecting its employees and found the problem wasn’t limited to certain age groups nor positions, markets, states, or even regions. “It’s very indiscriminate,” says the company’s head of human resources, Jennifer Carreon-Montes. “It’s affecting us, like it is our entire industry.”
In searching for the “why," looking over data and picking experts’ brains, something became unavoidably clear: The work and the nature of the business is a primary factor—if not the primary factor.
“We have more musculoskeletal injuries than a lot of other industries—roofing, but also remodeling in general,” Ribble says. “It’s physically demanding work. People tear rotator cuffs, get knee injuries, have back problems.” These types of injuries often require surgery, which is generally followed by a pain managementInjuries By The Numbers
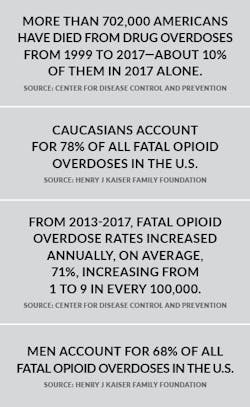
It’s well known that more people are hurt working construction jobs than most other occupations. The workplace incident rate is 13% higher than the average of other industries. Just working in construction is a risk.
But when you look at data specific to remodeling—roofing, siding, flooring, framing, etc.—those figures are extreme, even compared to overall construction, according the Bureau of Labor Statistics.
Roofing contractors, for instance, are injured more severely and at a rate 60% higher than workers in construction overall, and they’re more likely to injure multiple body parts. The situation for framers, with an incident rate 167% higher than the construction cumulative rate, is even worse. Of all the residential remodeling (and adjacent) verticals whose data we reviewed, only one had a lower incident rate than that of overall construction: finish carpenters. And their incident rate was still higher than the all-industries cumulative rate.
Under the simplest analysis, opioid abuse and addiction is a numbers game. The more injuries an industry has, the more doctor visits there are, and therefore the more chances for opioid prescriptions. So, relatively speaking, the odds are against remodelers.
The Nature Of The Business
“It’s the work” is an easy explanation for why opioids are plaguing remodeling. Severe injuries do, after all, abound. According to a survey of construction workers by The Center for Construction Research and Training, as many as a quarter have experienced injuries they didn’t report. So it’s likely injuries occur at an even higher rate than they appear. But that explanation only considers the nature of the work. It’s also the business itself.
“It’s physical labor, repetitive work, and there’s a culture of wanting to get back to work as quickly as possible,” says the National Association of Home Builders’ vice president of construction liability, David Jaffe, who also runs the association’s Opioid Working Group. Tradespeople want to get back to work so they can make money—hence not reporting injuries. They want to get back to work right away because if they don’t, the work may be done.
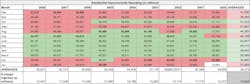
Residential remodeling is dependably seasonal. From October to January, spending falls consecutively month over month, according to our analysis of BLS data. That’s been true every year since the turn of the century. It’s also true that spending has risen month over month consecutively from March to June every year since the same time, with the exception of 2009. In the spring, spending is still low, but it rises through the summer and tends to stay high throughout the fall and into early winter, when it takes a big drop. Since 2015, the industry has averaged a 24% drop in remodeling spending during the slower season.
Healthcare Options
It’s a problem compounded by remodeling’s notorious lack of healthcare options for laborers, including paid sick leave, and the growing dependence on subcontractor labor that removes remodelers from the responsibility of healthcare completely. “It’s a trend that’s been not much spoken of over the last year, but it’s definitely happening,” says NRCA head Ribble. “The roofing industry is 40,000 workers short and to fill the gap, contractors are moving to subcontracted labor. Some are legal, some are not—hardly any have any sort of health plan.”
But even full-time employees aren’t guaranteed adequate health plans, or even paid sick leave. Data on insurance and paid sick leave in the remodeling industry is limited—a problem Pro Remodeler is attempting to correct with our biennial Wage & Benefits Study—but in our research, surveying nine of the country’s top remodeling markets, we discovered that: 1. Less than two-thirds of remodeling companies offer any sort of medical benefits; and 2. Seventeen percent of remodeling companies within those markets don’t offer any form of paid time off at all.
“Paid sick leave gives workers the freedom to heal on their own,” says Rachael Cooper, a senior program manager for Opioid Use Harm Prevention for the National Safety Council. “It reduces the need for a quick fix.” Opioids (or worse analogs, like heroin) are the quick fix to which she’s referring.
Opioid Addiction: A Systemic Problem
It may seem like the industry is not built to handle issues with opioids—and in a lot of ways, such as in its tradition of inadequate healthcare and reliance on subcontracted labor, it isn’t. It’s an issue so little spoken of in remodeling that David Jaffe referred to it as a “silent epidemic.” But the opioid issue, both in and out of industry, is a deep, systemic problem that’s less a reflection of preparedness than it is of general ignorance—even among the medical community.
It’s a problem compounded by remodeling’s notorious lack of healthcare options for laborers, including paid sick leave, and the growing dependence on subcontractor labor that removes remodelers from the responsibility of healthcare completely.
“Most medical providers receive very little education in pain, and even less education on addiction,” admits Yale’s Dr. Weimer, explaining that a widespread lack of understanding has resulted in doctors misprescribing or overprescribing pain medications, even when they’re not the most effective line of treatment.
“There’s really good evidence that the most effective treatment for back pain is active recovery,” Weimer says. “People shouldn’t really be using opioids for low back pain, but it’s one of the top reasons people go to their provider.” In Ohio, where construction workers are exceptionally at risk of opioid overdose, doctors in 2016 prescribed narcotic painkillers to 73% of injured workers.
The ignorance, she explains, stems from a lack of study and research on the subject. “Pain and addiction as a field of study is a relatively new thing.” It wasn’t until 2016 that the American Board of Medical SpecialtiesIt’s a frightening prospect, that our medical professionals might lack the understanding to effectively prescribe a drug that’s killing tens of thousands every year—and disproportionately killing people working construction. It’s part of the reason why Cooper suggests that businesses—remodelers in Ohio and Massachusetts and everywhere else—take it upon themselves to learn what it is that leads people to opioids, so that they can better prepare for it and speak to their employees about it. And maybe save someone’s life.
*Updated from "70,000" in our November print issue. The previous number reflects the number of total overall drug overdose fatalities in 2017.
About the Author

James F. McClister
James McClister is managing editor for Professional Remodeler.